What is Diabetic Neuropathy?
Diabetic neuropathy is a common and debilitating complication of diabetes that affects the peripheral nerves. The condition occurs due to prolonged exposure to high blood sugar levels, which can damage the nerves throughout the body. The peripheral nervous system is responsible for transmitting signals between the brain and spinal cord to the rest of the body, helping regulate sensations like pain, temperature, and touch. When these nerves are damaged, it leads to a range of symptoms and complications.
There are different types of diabetic neuropathy:
- Peripheral Neuropathy: The most common type, affecting the feet, legs, and sometimes the hands and arms.
- Autonomic Neuropathy: Affects nerves that control involuntary functions such as heart rate, digestion, and bladder control.
- Proximal Neuropathy: Affects the hips, thighs, or buttocks, leading to leg weakness.
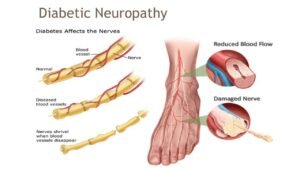
Although the exact mechanisms behind diabetic neuropathy are not fully understood, prolonged high blood sugar is considered a primary risk factor. Damage to the blood vessels that supply oxygen and nutrients to the nerves, as well as inflammation and oxidative stress, play significant roles in nerve deterioration.
What Causes Diabetic Neuropathy?
The primary cause of diabetic neuropathy is prolonged exposure to high glucose levels. Elevated blood sugar can damage nerves throughout the body, particularly in the hands and feet. Chronic hyperglycemia causes metabolic imbalances, impairing nerve function over time.
Other contributing factors include:
- Blood sugar fluctuations: Frequent spikes and drops in glucose levels can worsen nerve damage.
- Oxidative stress: High glucose levels increase the production of free radicals, which damage nerve cells.
- Inflammation: Chronic low-grade inflammation is another factor that exacerbates nerve damage in individuals with diabetes.
Maintaining stable blood sugar levels through diet, exercise, and medication is crucial to preventing or slowing the progression of diabetic neuropathy.
For tips on managing blood sugar, check out this resource from the Mayo Clinic.
Symptoms and Types of Diabetic Neuropathy
Diabetic neuropathy presents with various symptoms depending on the type of neuropathy affecting the individual:
- Peripheral Neuropathy:
- Symptoms: Tingling, numbness, burning pain, muscle weakness, and heightened sensitivity in the hands, feet, and legs. Patients may also have difficulty walking due to loss of coordination and balance.
- Autonomic Neuropathy:
- Symptoms: Dizziness upon standing (orthostatic hypotension), gastroparesis (delayed stomach emptying), digestive issues, and problems with heart rate and bladder control.
- Proximal Neuropathy:
- Symptoms: Weakness and pain in the hips, thighs, or buttocks. This form can make it difficult to stand or climb stairs.
- Focal Neuropathies:
- Symptoms: Sudden, severe pain in a specific area, such as the shin, or difficulty focusing the eyes due to damage to the eye muscles.
Recognizing these symptoms early is crucial for managing diabetic neuropathy and preventing further complications.
How is Diabetic Neuropathy Diagnosed?
Diagnosing diabetic neuropathy typically involves a combination of:
- Patient history: A detailed medical history, including diabetes management, symptoms, and duration of diabetes.
- Physical exam: Neurological evaluations such as reflex testing, muscle strength assessment, and sensitivity to touch or temperature.
- Specialized tests:
- Nerve conduction studies (NCS): Measure how quickly electrical signals travel through the nerves, helping to identify nerve damage.
- Electromyography (EMG): Evaluates muscle activity to detect nerve dysfunction.
- Blood tests: To check for glucose levels and other related complications.
Early diagnosis can help manage symptoms and prevent further nerve damage.
Treatment for Diabetic Neuropathy
There is no cure for diabetic neuropathy, but effective treatments focus on symptom management, slowing the progression of the condition, and preventing complications:
- Blood sugar control: The most important aspect of treatment. Proper diet, exercise, and adherence to prescribed medications are essential for preventing further nerve damage.
- Pain management:
- Medications: Pain relievers, anti-seizure drugs (e.g., gabapentin), or antidepressants like amitriptyline can help relieve pain.
- Topical treatments: Creams containing capsaicin or lidocaine can reduce localized pain.
- Physical therapy: Helps improve circulation, reduce pain, and maintain muscle strength. Regular exercise can also improve balance and mobility.
- Managing underlying conditions: Control of blood pressure, cholesterol levels, and weight is critical to minimizing further nerve damage.
Conclusion
Diabetic neuropathy is a significant complication of diabetes that can severely impact quality of life. Early intervention through proper diabetes management—such as blood sugar control, physical activity, and medication—can help reduce the risk of developing severe nerve damage. Regular check-ups and monitoring are essential for individuals with diabetes to catch the early signs of neuropathy.
In addition to traditional treatments, emerging therapies such as nerve decompression surgery and neuroprotective agents offer new hope for patients. Ongoing research and advancements in treatment options continue to provide optimism for managing this challenging condition.
For more information about managing diabetic neuropathy, visit the American Diabetes Association’s guide.

